A Guide to Assessing and Treating the Anterior Open Bite
Review anterior open bite case images, illustrations, patient evaluation checklist, and survey responses from DOT members.
Drag to resize
SHARE THIS

Unilateral cross-bites, bilateral cross-bites, deep bites, super-erupted teeth, roller-coaster bites…these are the dental and skeletal orthodontic cases that we all learned about while in dental school.
While there will be discussion, and even arguments, over the appropriate treatment for any of these types of dental malocclusions, there is another malocclusion that we see commonly in our dental practices that I did not learn about in my dental education that had me stumped during my early years in dentistry – the anterior open bite.
Malocclusion. This word to most dentists will invoke a variety of thoughts and visual scenarios. From the Class II bite (pic 1) with the retrognathic mandible to the Class III end-to-end occlusion (pic 2).
Pic 1
Pic 2
What is an Anterior Open Bite?
What is an Anterior Open Bite?
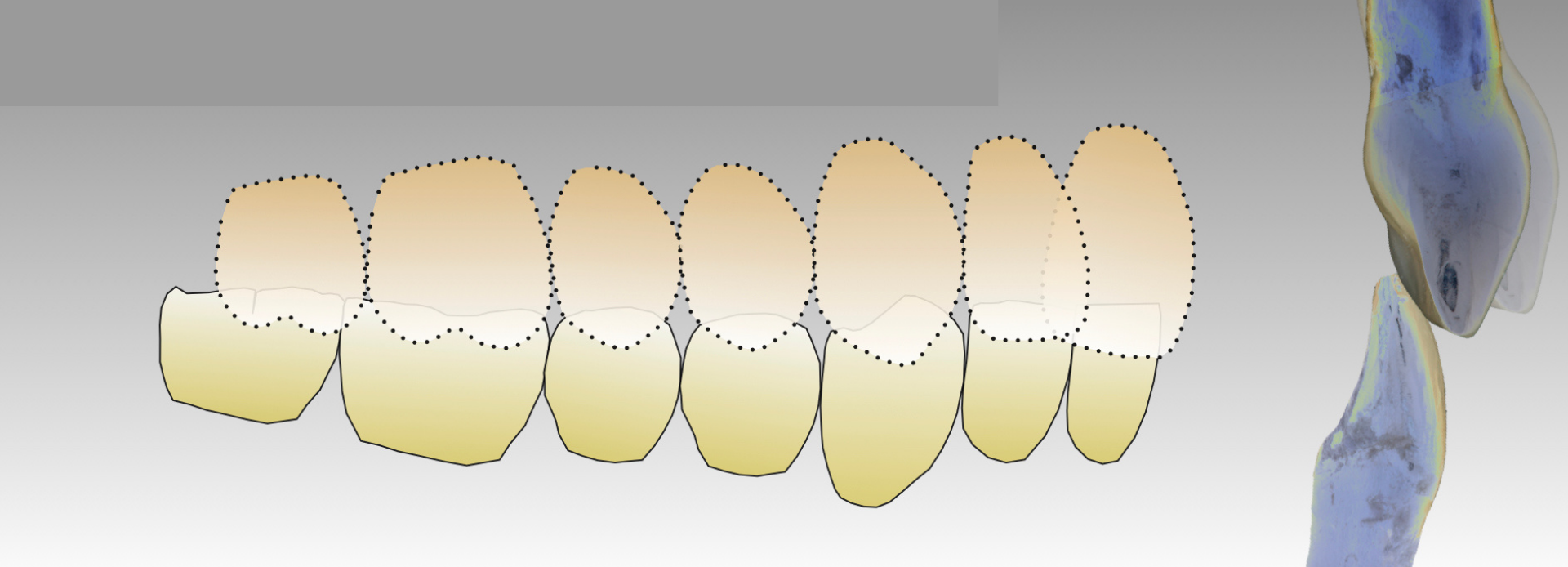
While anterior open bite cases can also be Class II malocclusions, these cases differ from the classic Class II cases because not only is there a horizontal discrepancy between the maxillary anterior teeth and mandibular anterior teeth, but there is also a vertical gap (see illustration 1, 2, 3).
Class I Occlusion - Illustration 1
Class II Malocclusion - Illustration 2
Anterior Open Bite - Illustration 3
In fact, in a Class II, division II case, there is commonly contact with the maxillary and mandibular incisors as the central incisors have become palatally tipped (illustration 4). So, indeed, anterior open bites can be in any occlusal relationship – Class I’s, Class II’s, and Class III’s.
Class II Malocclusion - Div 2 - Illustration 4
So, over the years, I’ve been wondering - why with some patients do we see a gap between the upper and lower front teeth? We’re taught that teeth are supposed to erupt until they come in contact with an opposing tooth, and in the anterior dentition, if the bite is not stable, the teeth will over-erupt, or super-erupt creating a deep bite. So why aren’t the front teeth coming together with these anterior open bites?
Correcting these anterior open bites can be challenging for the orthodontist. Try as they may, some of the open bites just don’t seem to want to close. Orthodontists I have worked with would typically consider that the patient has a strong tongue thrust, or forward tongue posturing habit, that would prevent the closing of these open bites with orthodontics.
What Causes the Anterior Open Bite?
With these tongue thrust/positioning habits, we’ll see patients with their tongue resting between their anterior teeth, and if the tongue is there, then the teeth can’t be moved into that space. This theory makes pretty good sense – the tongue is an incredibly strong muscle, and as Dr. Peter Dawson once said, “when teeth and muscles battle, muscle wins.”
When teeth and muscles battle, muscle wins.
- Peter Dawson, DDS
Orthodontists even go so far as to bond sharp prongs onto the lingual of the maxillary anterior teeth to keep the tongue from coming forward against the anterior teeth. But still, the orthodontists are often thwarted in their attempts to close these anterior open bites.
Frequently, myofunctional therapists are enlisted to coach patients on proper tongue position to help the orthodontist align the teeth appropriately. This functional therapy can help the patient learn techniques to get the tongue out of the way.
I keep wondering, why does the patient position their tongue forward? And, here’s a question, is this the chicken and the egg scenario? Has the tongue positioning caused the separation of the anterior teeth, or is it possible, that there is an anterior open bite and the tongue has moved into the position not occupied by the teeth? Hmmmmm!
Can we Correct the Anterior Open Bite?
In author Dan Heath’s book – ‘Upstream: The Quest to Solve Problems Before They Begin’, Dan gives the following dramatization:
You and a friend at a river when you notice a child drowning, in need of rescuing. No sooner do you grab the child from the river when another child is heading towards you, also in need of rescue. This happens again and again. The two of you can barely keep up. Suddenly, you see your friend wading out of the water, seeming to leave you alone. “Where are you going?” you demand. Your friend answers, “I’m going upstream to tackle the guy who’s throwing all these kids in the water.”
You and a friend at a river when you notice a child drowning, in need of rescuing. No sooner do you grab the child from the river when another child is heading towards you, also in need of rescue. This happens again and again. The two of you can barely keep up. Suddenly, you see your friend wading out of the water, seeming to leave you alone. “Where are you going?” you demand. Your friend answers, “I’m going upstream to tackle the guy who’s throwing all these kids in the water.”
This story, and ‘Upstream’ had me thinking about these pesky anterior open bites, and our understanding and treatment of them. Maybe, just maybe, there are times that the tongue thrust, or perhaps more appropriately, the tongue posturing, is secondary to the open bite.
Maybe the tongue isn’t causing the separation of the maxillary and mandibular anterior teeth in some cases. Maybe the tongue is just occupying the space that is there. To consider this alternative explanation for the anterior open bite, we need to look beyond just the teeth and how they fit together.
We need to evaluate the entire occlusal complex; that’s right, we need to look at the entire maxillo-mandibular system – we need to go upstream – to the TM joint.
We need to evaluate the entire occlusal complex; that’s right, we need to look at the entire maxillo-mandibular system – we need to go upstream – to the TM joint.
Temporomandibular Joint & the Anterior Open Bite
In illustration #5, we see a healthy-shaped condyle in the appropriate position in the condylar space with a disc separating the condyle from the fossa. The teeth are interdigitated in a Class I occlusion.
Class I - Illustration 5
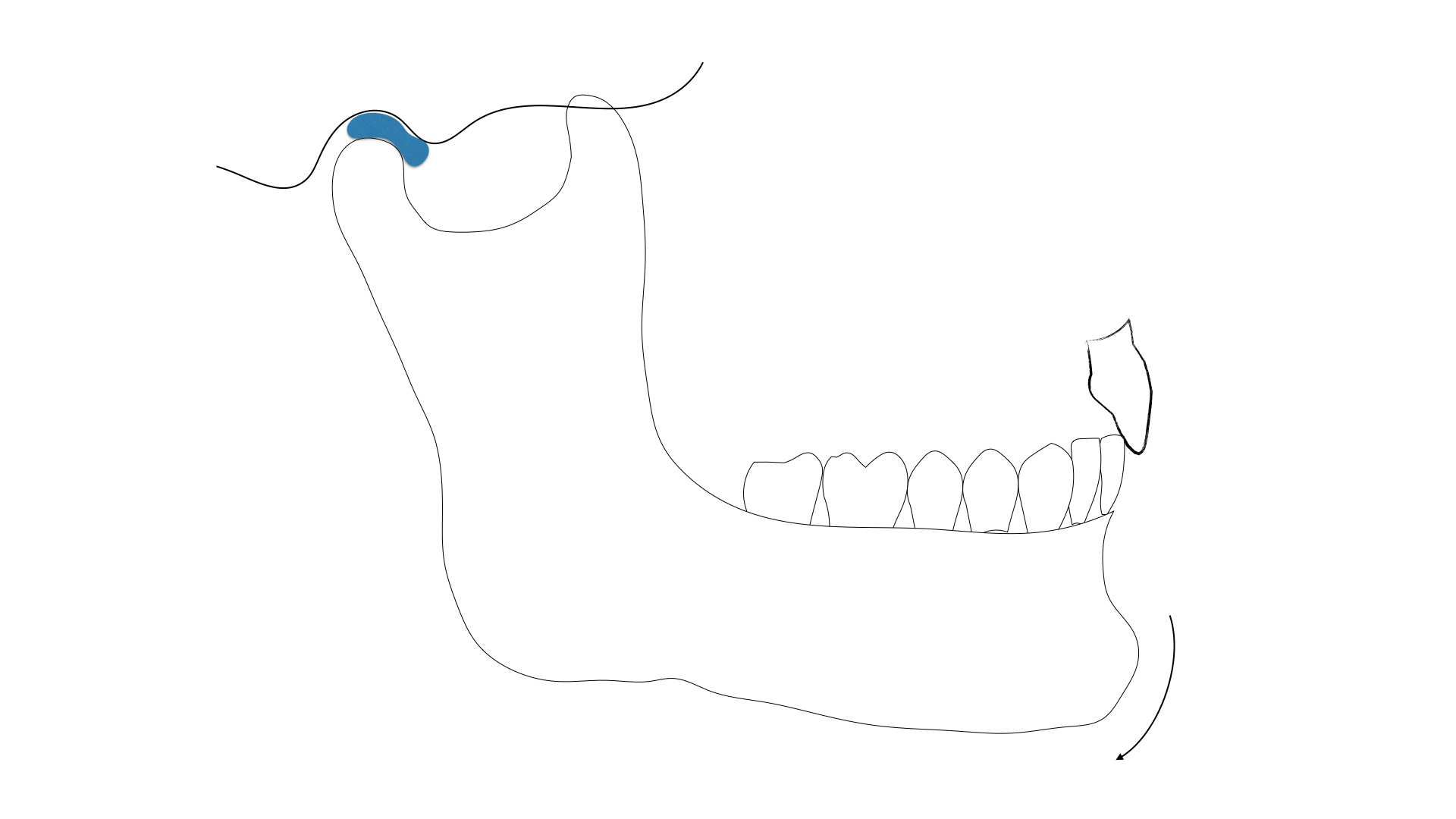
This is the ideal world – teeth in the proper position with the joints seated appropriately in the joint space with the disc separating the bones. Now imagine that the disc has displaced, or degenerated.
While traditional dental training will make this seem far-fetched, and rare in occurrence, I will tell you that in my practice, this is not uncommon. We see patients with displaced, or herniated discs, routinely. Most patients are asymptomatic, or their complaints are minimal and easily managed by the patient.
While some patients are referred for TMD issues because of pain, most people are able to manage and tolerate pain with little concern.
While some patients are referred for TMD issues because of pain, most people are able to manage and tolerate pain with little concern.
Class I - Illustration 6
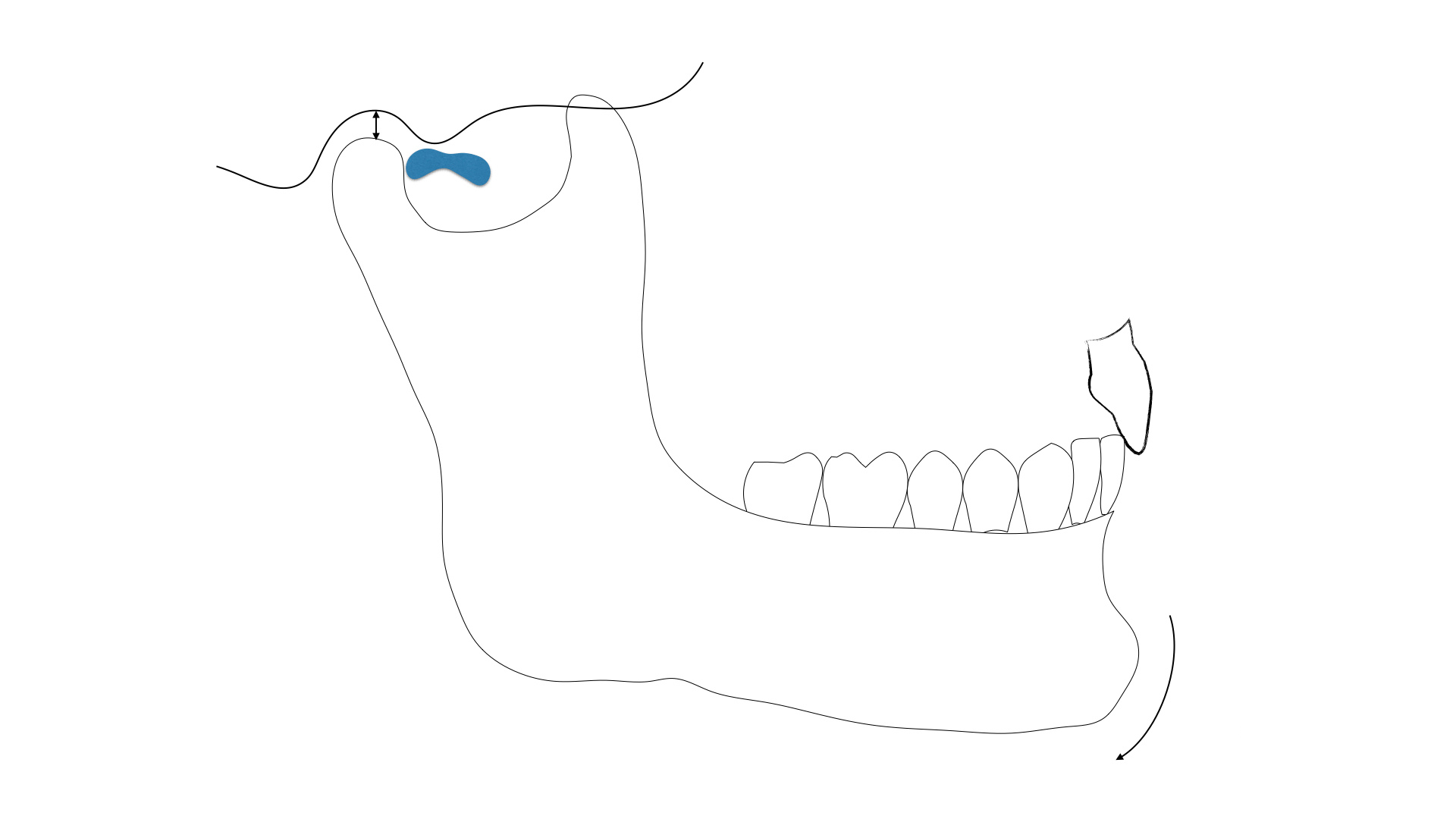
In illustration 6, we are ‘displacing’ the disc, in which the disc will be pulled forward, or anterior to the condyle. The space that the disc was occupying (approximately 3 mm thickness), will not stay unaltered. Unless there is an immediate filling in of this space with retrodiscal tissue, the condyle will rotate upward to fill the space (Illustration #7). As the condyle moves upward to fill the space, there is a clockwise rotation of the mandible. As the condyle rotates clockwise, the posterior teeth will contact but the mandibular anterior teeth will separate from the maxillary anterior teeth (illustration #8).
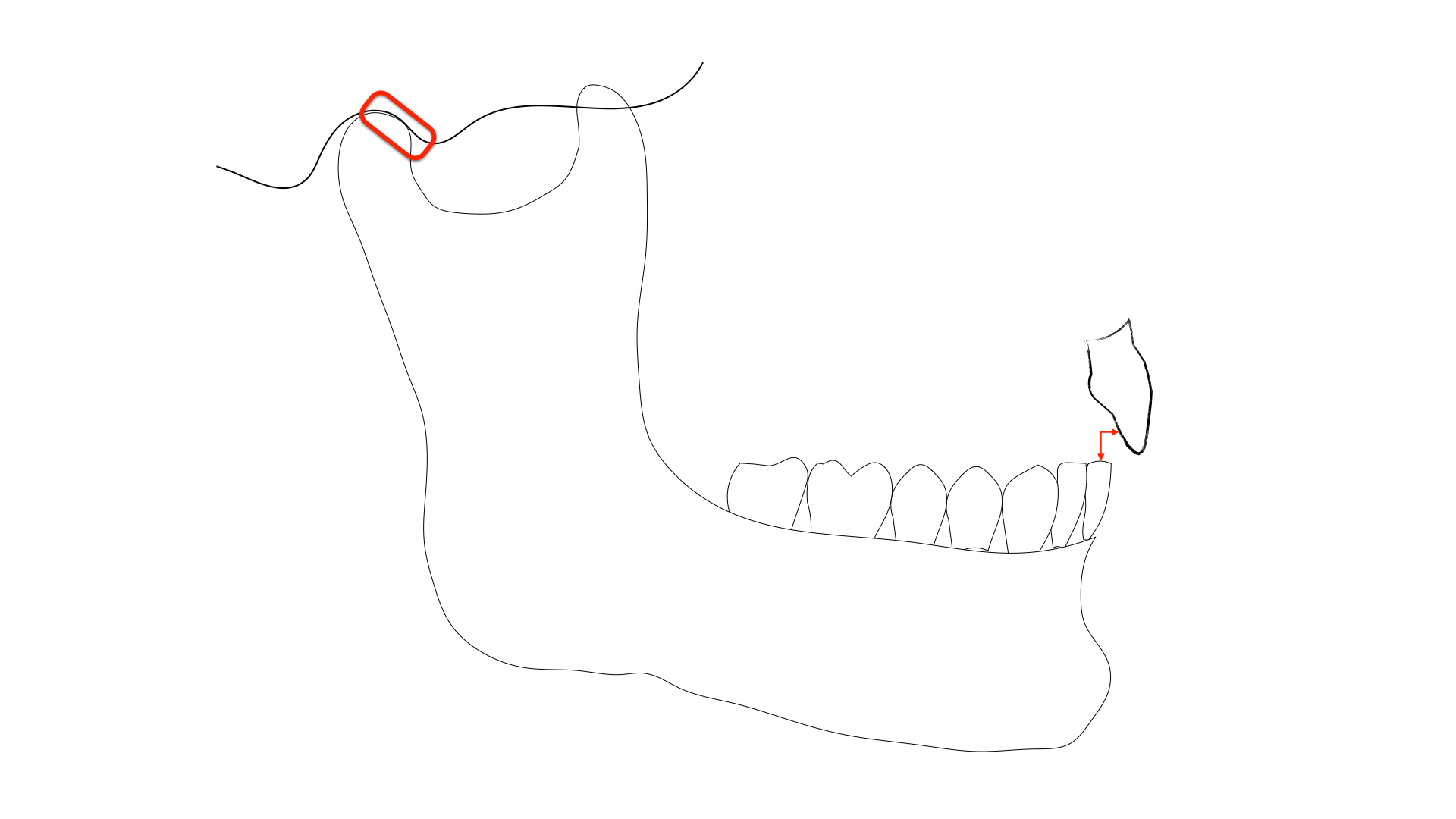
As you look at this illustration, can you imagine how this could result in an anterior open bite? Would you agree that it’s certainly one possibility? After evaluating a tremendous number of MRI’s of patients with anterior open bites, they all, yes all, have displaced discs.
After evaluating a tremendous number of MRI’s of patients with anterior open bites, they all, yes all, have displaced discs.
I have learned this information from many dental colleagues over the years, most notably, occlusion expert, Dr. Jim McKee.
The main thing with anterior open bites is to determine whether or not they are getting more open over time (active degeneration vs stable joints). It is very difficult to get a diagnostic MRI from medical providers... Without the imaging, you are just guessing what will work. Either it's muscle and occlusal interference, where anything will work; or it's joint disease and likely anything like splint therapy, ortho, equilibration, or restorative work will fail if the joint is not stable.
RANDY VALENTA, DDS
DOT Premium Member, Survey Response
Orthodontic Treatment of the Anterior Open Bite
Let’s say that the open bite is related to displaced discs or changes in the condylar space. Why don’t the anterior teeth erupt to contact the opposing anterior teeth? What keeps the orthodontist from getting the anterior teeth to fit together?
Some patients with bad TM joints need to support their joints to create some stability or a comfortable resting position. These patients, in order to reduce pain or soreness, will position their tongue to fill the gap between the front teeth to give more occlusal support. This tongue resting position may simply be enough to help improve their comfort.

Imagine a patient going through orthodontics and finding relief with forward tongue posturing. It will likely be impossible for the orthodontist to bring the anterior teeth together if the tongue wants to maintain the space to reduce stresses in the TM joints. Palatal pronges and myofunctional therapy may help, but if the patient has sore or painful joints, the need to reduce the joint pain may overcome these other tools used by the orthodontist.
Now, like most things in life, I don’t believe that there is just one answer to this issue. There are two other types of patients to consider with the anterior open bite that may not have been on our radar previously.
Moving beyond the TMJ patient, another type of anterior open-bite patient requiring consideration may be the airway patient.
Airway & the Anterior Open Bite
We are learning more and more about patients whose airways are compromised, and the effect on their dental conditions. For some patients, as we have discussed in detail in our CPR for the Worn Dentition Course, bruxism, erosion, and tooth wear can be significant issues. Other patients may present differently.
Obviously, there is a discussion about sleep quality and evaluation of bruxism as part of this regardless of joint symptoms. These patients tend to be the ones that have worn/cracked lower second molars that, when prepped for full coverage, allow the joint to seat and you lose your occlusal clearance. At this point, after going through your cpr for worn dention, I'd feel much more comfortable proceeding restoratively with no ortho, if patient had no joint symptoms and was satisfied with overall tooth alignment.
DOT Premium Member, Survey Response
Write your awesome label here.
In this clip from our CPR for the Worn Dentition Course, Dr. Hartlieb reviews the causes of tooth erosion and the screening protocol he uses for patients with wear.
Patients that are challenged to breathe through their nose will choose to breathe through their mouths instead. There is strong research that suggests that nasal breathing is critical for optimal health, but for patients that have allergies, deviated septums, clogged or narrow nasal passages, or collapsible nares - these patients may not be able to breathe through their nose.
If these patients also have large tonsils and adenoids or are simply biologically designed to have a narrow airway (this can be visualized with a CBCT), they may find it difficult to breathe even through their mouth. To allow adequate airflow, these people will position their mandible and tongue forward to get more air. They literally may need to protrude their tongue forward to lift the base of the tongue out of the back of the throat.
As dentists, we know these patients all too well. They’ll often appear as narrow, high vaulted palate patients. They are our gaggers. These are the patients that make us feel like we just wrestled with an alligator after treating a posterior molar. If you stand back, you might notice that many of these patients will posture their heads forward and a little downward – this positioning helps them with their breathing. When the person sits upright, their airway becomes compromised. These are our airway patients.
Evaluate for tongue thrust. Consider sleep study to evaluate for OSA as patient may be subconsciously moving tongue forward to open up airway to breathe better.
DARREN G. KOCH, DDS
DOT Premium Member, Survey Response
So, I think you can imagine that if a person needs to position their tongue forward to help them breathe, a forward tongue posturing position could easily result in an anterior open bite. The bottom line is if the person needs that forward tongue position to breathe, good luck trying to move the teeth into a position that will block the tongue!
Tongue-Tie & the Anterior Open Bite
Another concept that I have become aware of only recently is the effect of tongue-tie on our maxilla development and our dental occlusions.
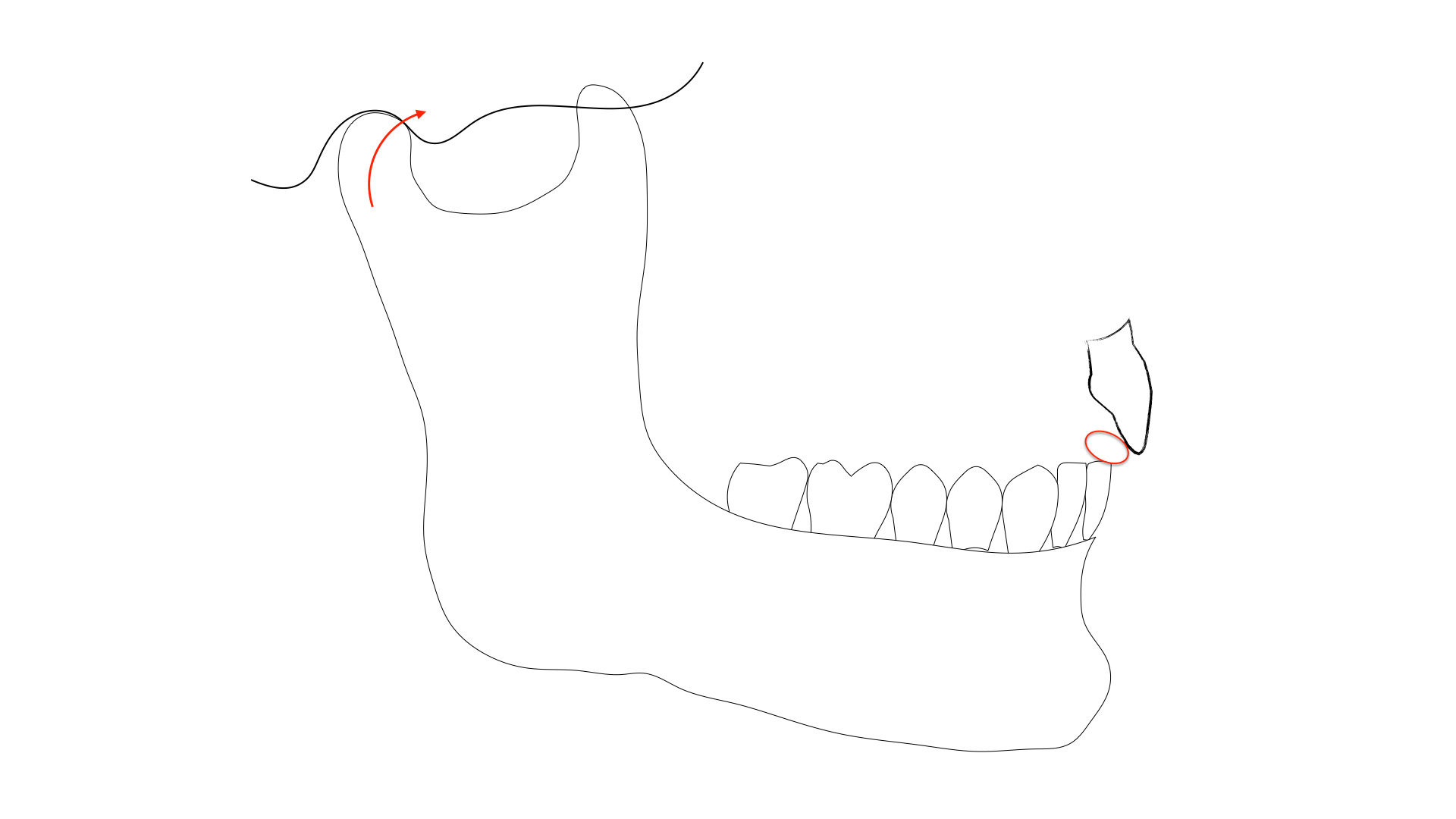
If a patient with a severe tongue-tie is not able to allow their tongue to rest in a normal position against the anterior and posterior palate, and the tongue is maintained forward during swallowing due to the tongue tie, this could also affect the interarch anterior tooth positioning (pic 3).
If a patient with a severe tongue-tie is not able to allow their tongue to rest in a normal position against the anterior and posterior palate, and the tongue is maintained forward during swallowing due to the tongue tie, this could also affect the interarch anterior tooth positioning (pic 3).
Pic 3

The anterior positioning of the tongue could affect the ability of the orthodontist to gain ideal tooth positioning as the tongue fights for the space. Early recognition and treatment are critical for these patients and should be identified by pediatricians and lactation consultants with infants during nursing.
If not identified during infancy, pediatric dentists, general dentists and speech pathologists should identify potential issues during their oral examinations. The earlier the tongue tie is treated, the more likely the patient will develop appropriate maxilla and mandibular development (if all other anatomical features are normal), proper swallowing patterns, and normal tooth positioning.
Anterior Open Bite Patient Evaluation Checklist:
Ask yourself the following questions when a patient presents with an anterior open bite in your practice:
-
Is this a TM joint patient who should have imaging of their joints to check for disc health?
-
Is this an airway patient with compromised nasal breathing, narrow maxilla, poor airway anatomy?
-
Should this type of patient be evaluated for airway obstruction issues?
-
Should an ENT referral be considered to see if we can help the patient breathe better through their nose?
-
Is the lack of palatal development, and with it the base of the nose, related to a tongue tie?
-
Is swallowing compromised in these patients and a forward tongue posture secondary to the tongue tie?
-
Should a consultation with a myofunctional therapist be considered to improve tongue posturing and function?
Survey Results
Survey Results
We asked DOT members several questions on treatment planning for the anterior open bite. Check out the results!

If the anterior open bite patient has no joint pain, and no esthetic or functional concerns, which best describes your first course of action?
Monitor and Maintenance (70.8 %)

Orthodontic referral (37.5%)
Mounted study casts to evaluate further (12.5%)

Joint imaging (CBCT and/or MRI) (4.2%)
Nightguard or bite splint (4.2%)
Other (4.2%)
"ortho retention appliance to prevent super eruption of mandibular anterior teeth"
If the anterior open bite patient HAS TM joint pain, which would likely be your treatment recommendation:
Orthodontic referral (56.5%)

Joint imaging (CBCT and/or MRI) (39.1%)
Nightguard or bite splint (34.8%)
Equilibration (8.7%)
Other (4.3%)
"Oral Surgeon referral."
If the patient HAS NO TM joint pain but is dissatisfied with the appearance of their smile, which of the following would you include in your treatment recommendations?
Orthodontics (95.7%)

Restorative treatment (56.5%)

Orthognathic surgery (39.1%)
Joint imaging (CBCT and/or MRI) (21.7%)
Other (4.3%)
"photos, mounted models, trial equilibration, if unsatisfactory results on the model then send to ortho."

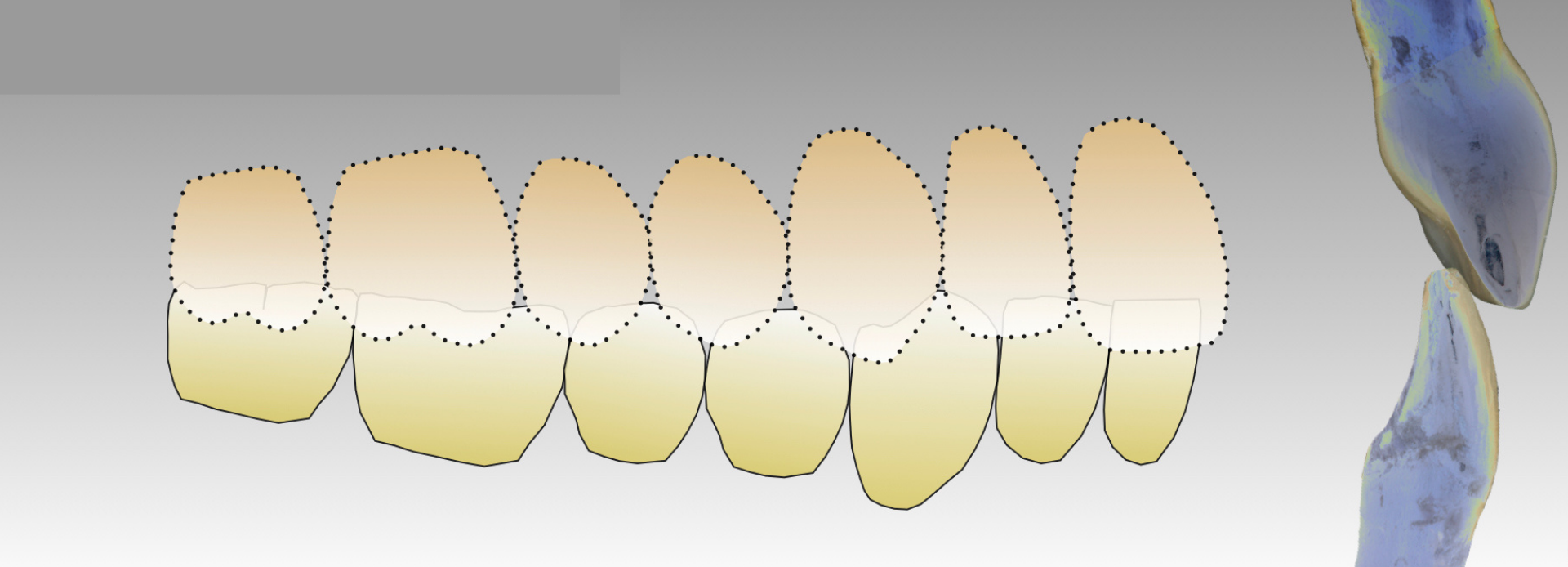
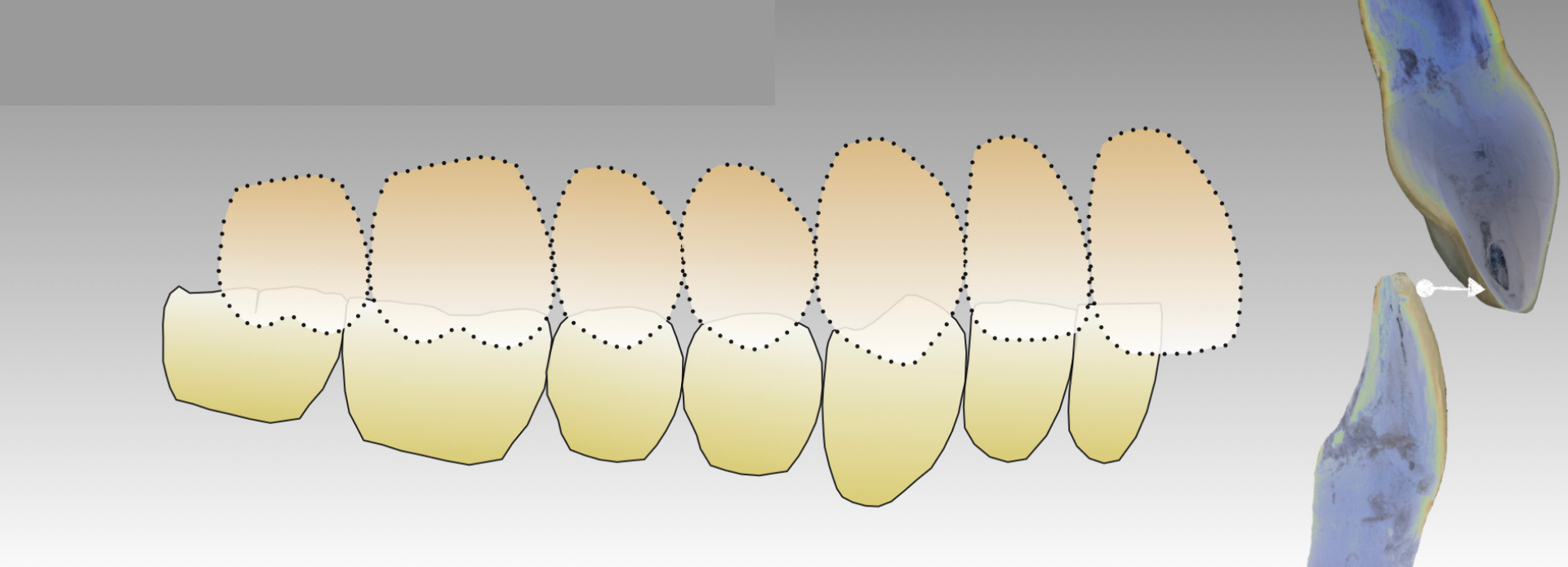
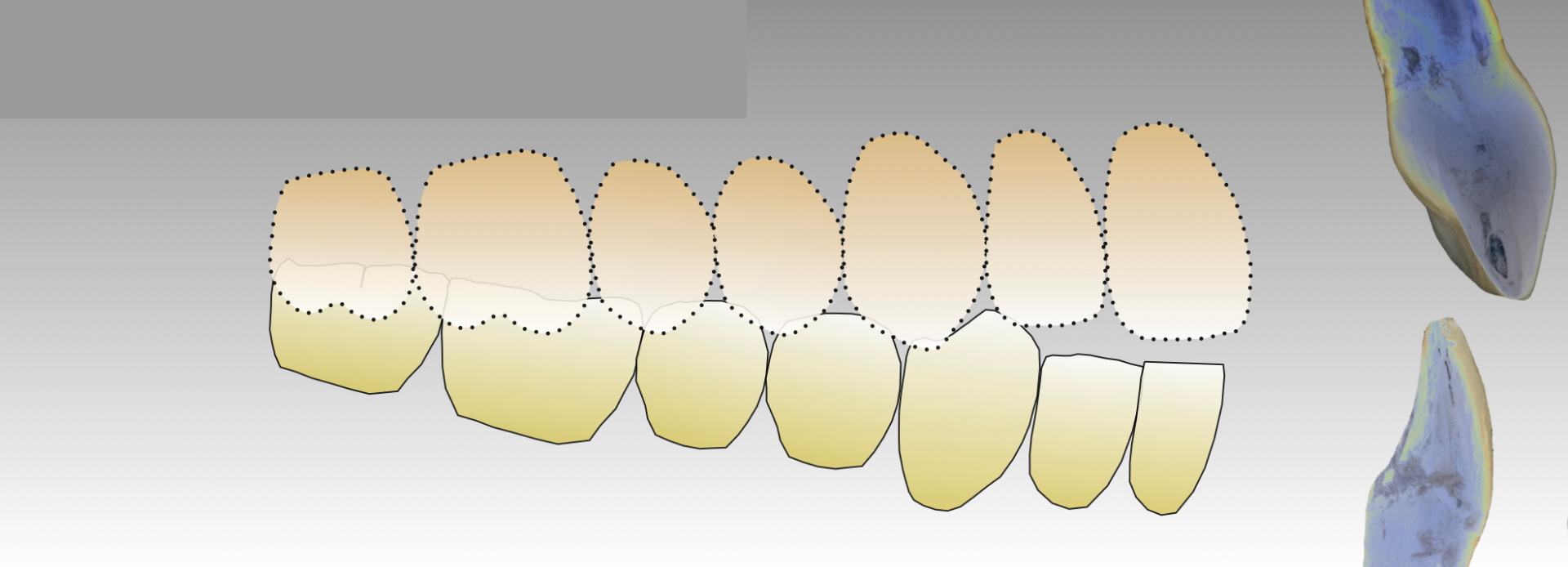
The patient in the photograph has two bites, an MIP where all the teeth fit together and a seated joint position bite where only posterior teeth touch.
If the patient has no TM joint pain, what would be your likely first recommendation to the patient?
Monitor and Maintenance (75%)

Mounted study casts to evaluate further (37.5%)
Orthodontic referral (29.2%)
Joint imaging (CBCT and/or MRI) (4.2%)
Nightguard or bite splint (4.2%)
If the patient does have TM joint pain, what would be your likely first recommendation to the patient?
Mounted study casts to evaluate further (50%)
Nightguard or bite splint (37.5%)
Orthodontic referral (37.5%)
Joint imaging (CBCT and/or MRI) (33.3%)
Monitor and Maintenance (4.2%)
Final Thoughts...
Final Thoughts...
Maybe there are additional explanations for the anterior open bite that we haven’t explored, identified, or discovered. So often in life, as we learn more, we find that we know less.
Indeed, anterior open bites were not even on my radar as a young dentist, but as I began to see them, I began to wonder “why?”
I don’t see anterior open bites in practice every day. This is not an ‘every patient’ issue…but it does remind me in a way of peg lateral cases. Peg laterals make up only about 2-2.5% of our population, but we need to be able to treat them when they do show up in our office.
With these anterior open bite cases, consider the TM joints, the nasal passages, and the tongue prior to trying to correct the problem. Let’s do our best to find an accurate diagnosis – it may be more than one – and then look ‘upstream’ as we develop the appropriate treatment plan for the optimal long-term health of our patients!
Yours for better dentistry,
Dennis B. Hartlieb, DDS, AAACD
Drag to resize
Related courses:
→ A New Perspective on Occlusion and TMD with Dr. Jim McKee
→ Reading MRIs - Let's Look Inside
→ The Airway Patient in Your Dental Practice
→ Reading MRIs - Let's Look Inside
→ The Airway Patient in Your Dental Practice
Drag to resize
Dennis B. Hartlieb, DDS, AAACD
DOT Founder
Share this page
Join 10,000+ dentists who get tips bi-weekly.
Thank you!
By signing up you agree to our Privacy Policy.
Latest from our blog
Our vision is to provide online continuing education workshops and mentorship that are comprehensive for dentists learning at all career levels. DOT is developed for dentists that love to learn online.
CONNECT
Materials Included
Light Brown tints, Enamelize, Unfilled Resin Flexidiscs, Flexibuffs 1/2", #1 artist’s brush, Silicone Polishing Points, IPC Off Angle Short Titanium Coated Composite Instrument
Materials Needed, not Included
- Loupes
Follow along
You are Registered
We’re excited to have you join us! You’ll receive email reminders at with the link to join this event.
If you have any questions in the meantime, feel free to reach out to us at dot@dothandson.com—we’re here to help!
Day 1 (8 - 4 pm CST)
-
Erosion and wear – the why and the how
-
Adding length to teeth – when is it safe
-
Opening VDO to compensate for lost tooth structure – where to begin
-
Records visit and key points you need to understand before you start
-
The smile – the 7 strategic points to consider when evaluating the smile
-
Anterior tooth shape, morphology
-
Clinical case review
-
Upper Putty matrix construction
-
Build lingual incisal wall with putty matrix #6 - #11/ Upper anteriors
-
Full contour build-up #6, #7, #8, #9, #10, #11, shape and polish/ Upper anteriors
Day 2 (8 - 2 pm CST)
-
Who – which patients are candidates
-
Why – explaining to patients the value of the prototype
-
How – step-by-step techniques to maximize predictability, efficiency and success
-
Getting to Yes: conversations with patients about esthetic and reconstructive dentistry
-
The ‘Smile Preview’ – techniques to show the possibilities
-
Lower Putty matrix construction
-
Build lingual incisal wall with putty matrix #22 - #27 / lower anteriors
-
Build-up #22 - #27, shape and polish / lower anteriors
-
Build-up lower occlusal posteriors
-
Demonstration of Smile Preview
Upcoming Virtual Workshops
Write your awesome label here.
December 11 & 12, 2025
CPR for the Worn Dentition (16 CE)
Write your awesome label here.
January 29-30, 2026
Porcelain Veneer Cementation Workshop (14 CE)
Write your awesome label here.
March 27, 2026
Esthetic and Functional Success for Diastema Closure (8 CE)
Write your awesome label here.
May 15, 2026
From Break to Beautiful: Flawless Class IV Resin Restorations (8 CE)
Write your awesome label here.
June 19, 2026
Mastering Intraoral Scanners and Digital Workflow for the Dental Team (4 CE)
Write your awesome label here.
September 25, 2026
Veneering the Dark Central Incisor - Conservative Direct and Indirect Restorative Strategies (8 CE)
Write your awesome label here.
October 30, 2026
3D Printing for the Restorative Dentist
Write your awesome label here.
December 11, 2026
Injection Molding Workshop (8 CE)
Write your awesome label here.
Study Club
Join five in-depth virtual meetings held on Thursday evenings throughout the year. Engage in detailed case presentations, discuss curated research articles, and exchange valuable tips with fellow dentists.
-
01/22/2026
-
04/09/2026
-
06/11/2026
-
10/15/2026
-
12/10/2026
Write your awesome label here.
Coffee & Donuts
Kickstart your Friday mornings with informal sessions and discuss patient treatments, practice management, and receive feedback on your cases.
-
01/16/2026
-
02/13/2026
-
03/20/2026
-
04/10/2026
-
05/08/2026
-
06/05/2026
-
08/21/2026
-
10/09/2026
-
11/20/2026
-
12/10/2026
Popular On-Demand Courses
Write your awesome label here.
Injection Moulding Techniques (3 CE)
Simple, predictable, systematic foundation for you to start your journey with injection moulding
Write your awesome label here.
Advanced Techniques in Composite Veneers (6 CE)
Take control of aesthetic cases in your practice, whether you are enhancing smiles with direct resin veneers or creating provisional restorations for indirect cases.
Write your awesome label here.
A Realistic Perspective on Occlusal Appliances (3 CE)
Learn how to design, fabricate, and manage occlusal appliances with confidence through practical guidance and real clinical case examples.
Write your awesome label here.
Bicuspid Veneer and V-Onlay Preparation (3 CE)
Gain expertise in ‘prep-less’ veneers, buccal cusp reduction, and margin placement methods to enhance your clinical outcomes.
Write your awesome label here.
Class IV Composite Restoration – Polychromatic Approach (3 CE)
This on-demand course covers material selection and advanced layering techniques to help you create natural-looking, long-lasting restorations that set you apart.
Write your awesome label here.
EXOCAD: Foundation (2 CE)
Gain the skills to confidently navigate Exocad, build patient cases, and streamline your workflow using time-saving techniques and presets.
Write your awesome label here.
Class II Direct Resin (3 CE)
Master a reliable approach to Class II restorations by learning how to create ideal proximal contacts that enhance both the strength and aesthetics of your work.