Written by Dr. Dennis Hartlieb
Case Study: TMJ Splint Therapy and Prototype Bonding for the TMD Patient
Many cosmetic patients have underlying joint issues. Review a complete guide to evaluate and manage temporomandibular disorders and how to use TMJ splint therapy to successfully manage discomfort.
Drag to resize
(Read time 7-9 minutes)
What are Key Indicators of TM Joint Issues?
For many years in my dental practice, I was under the impression that most of the patients that I treated had healthy Temporomandibular joints (TM joints). Patients rarely complained of joint issues, or if there were any complaints, they generally were mild, non-severe issues, some of which include:
Common TMD Patient Complaints
-
Patient has a sore jaw
-
Patient says their jaw makes a clicking sound when chewing
-
Patient complains of jaw muscles being tired
-
Patient has a history of being unable to open mouth completely or partially
As a young dentist, these non-descript anecdotes were easy to ignore and overlook. This belief I had falls under the “You only see what you know, and you only know what you can see” mantra.
When I did see patients that had any type of TMJ disorders, I assumed that they were muscular based, probably related to the patient’s clenching and grinding of their teeth.
When I did see patients that had any type of TMJ disorders, I assumed that they were muscular based, probably related to the patient’s clenching and grinding of their teeth.
Write your awesome label here.
TMD Patient Webinar: Dr. Hartlieb reviews what a healthy TMJ looks like
Managing TMJ Issues with a Night Guard
For a long time, I never used TMJ splint therapy and I treated all my patients that had TMD symptoms with a night guard with the belief that if I could control the patient’s bite forces during sleep, I would be able to reduce their TMD issues, most notably TM joint pain and headaches.
I didn’t worry about the patient’s joint position – we simply had the lab hand-articulate the cases (maximum intercuspation) rather than worry about finding their centric relation bite, and mounting the cases on a semi-adjustable articulator.
I didn’t worry about the patient’s joint position – we simply had the lab hand-articulate the cases (maximum intercuspation) rather than worry about finding their centric relation bite, and mounting the cases on a semi-adjustable articulator.
For many patients, an appropriately balanced night guard was very helpful in bringing patients comfort. However, there were patients that did not respond well to their night guards.
Some patients would report that they would take their night guard out at night while sleeping, without even realizing it. Often the patient would say that the night guard “fell out” while they were sleeping, but somehow magically it ended up on their nightstand, or under their pillow.
I’ve come to understand that with TMD patients, there is likely an airway element, or a sleep disordered breathing issue underlying their nighttime bruxism.
Evaluation for obstructive sleep apnea should be considered with these patients that fail treatment with a traditional night guard.
Some patients would report that they would take their night guard out at night while sleeping, without even realizing it. Often the patient would say that the night guard “fell out” while they were sleeping, but somehow magically it ended up on their nightstand, or under their pillow.
I’ve come to understand that with TMD patients, there is likely an airway element, or a sleep disordered breathing issue underlying their nighttime bruxism.
Evaluation for obstructive sleep apnea should be considered with these patients that fail treatment with a traditional night guard.
What if a Patient Fails Night Guard Therapy?
Another type of patient that fails night guard therapy, is one whose symptoms do not improve while wearing their night guard. These are patients whose symptoms not only do not seem to improve, but actually may worsen with the use of the night guard.
These patients typically, in my experience, were those that had reported with a history of clicking or popping TM joints, a history of limited opening or jaw locking, or other symptoms that would be considered beyond just muscular issues.
These are patients that need a more comprehensive evaluation that may include imaging with CBCT, and with MRI.
As crazy as it may seem, I have found many of my general restorative patients, and many of my cosmetic patients, have underlying joint issues. These patients, in an effort to provide long-term restorative or cosmetic success, very often need TMJ stability, prior to their actual restorative treatment.
I have felt for many years that in order to get a strong foundation in cosmetics, you must first get a strong foundation in occlusion.
These patients typically, in my experience, were those that had reported with a history of clicking or popping TM joints, a history of limited opening or jaw locking, or other symptoms that would be considered beyond just muscular issues.
These are patients that need a more comprehensive evaluation that may include imaging with CBCT, and with MRI.
As crazy as it may seem, I have found many of my general restorative patients, and many of my cosmetic patients, have underlying joint issues. These patients, in an effort to provide long-term restorative or cosmetic success, very often need TMJ stability, prior to their actual restorative treatment.
I have felt for many years that in order to get a strong foundation in cosmetics, you must first get a strong foundation in occlusion.
I have felt for many years that in order to get a strong foundation in cosmetics, you must first get a strong foundation in occlusion.
Today’s blog is a look at how a patient that presents with cosmetic needs, but also has TM joint breakdown, is managed, and how prototype bonding is critical in the patient’s restorative and cosmetic success.
The Onion and the TMD Patient
Write your awesome label here.
TMD Patient Webinar: How is the TM Joint like an onion?
I was taught that the best way to consider TMD, is to consider the TM joint as an onion.
If we slice the onion and look at the rings inside, the outermost rings relate to the most prevalent symptom of TMD – muscle issues. As discussed above, we are often able to manage TMD patients by reducing their muscle intensity during clenching and grinding with an appropriately adjusted night guard.
There are many different night guard designs that can be affective – upper or lower full arch splints or anterior deprogrammers such as an NTI* appliance have all proven to be successful in reducing muscle activity with nocturnal bruxers. The critical factor with these splints is that they all prevent the posterior teeth from touching when the patient moves their jaw in eccentric movements.
If we slice the onion and look at the rings inside, the outermost rings relate to the most prevalent symptom of TMD – muscle issues. As discussed above, we are often able to manage TMD patients by reducing their muscle intensity during clenching and grinding with an appropriately adjusted night guard.
There are many different night guard designs that can be affective – upper or lower full arch splints or anterior deprogrammers such as an NTI* appliance have all proven to be successful in reducing muscle activity with nocturnal bruxers. The critical factor with these splints is that they all prevent the posterior teeth from touching when the patient moves their jaw in eccentric movements.
As I stated in the beginning of this blog, my belief in my early days of treating patients was that most patients with TMD were related to muscle issues. As I have been practicing dentistry longer and longer, I believe that there are probably an equal number of patients with TMD issues that are beyond just muscular pain issues – those with issues within the joint.
If we consider the onion analogy, as we peel back the onion, we now consider the second layer of TM disorder, the TMJ disc. These patients have generally been ignored in dentistry – these are the patients that have clicks or pops in their jaw joints, or patients that have had a history of limited opening or times when their jaws are ‘locked’.
As dentists, we typically tell the patient that the clicks are normal, and advise them to beware of biting into too hard of foods, or limit gum chewing.
When examined closely, these patients will often present with two different bites – one bite when they bring their teeth together, and one when the condyles are seated. The first bite, the bite where the patient is able to bring their teeth together, is referred to as maximum intercuspation, or MIP (formerly centric occlusion for us older docs).
If we consider the onion analogy, as we peel back the onion, we now consider the second layer of TM disorder, the TMJ disc. These patients have generally been ignored in dentistry – these are the patients that have clicks or pops in their jaw joints, or patients that have had a history of limited opening or times when their jaws are ‘locked’.
As dentists, we typically tell the patient that the clicks are normal, and advise them to beware of biting into too hard of foods, or limit gum chewing.
When examined closely, these patients will often present with two different bites – one bite when they bring their teeth together, and one when the condyles are seated. The first bite, the bite where the patient is able to bring their teeth together, is referred to as maximum intercuspation, or MIP (formerly centric occlusion for us older docs).
CLASS II - MAXIMUM INTERCUSPATION
MIP relies on the muscles of mastication to coordinate in order to bring the mandible into a desired position to maximize the number of teeth that touch while closing, or chewing. This is the patient’s ‘normal’ bite – when we ask the patient to bite together, this is their MIP.

The second bite is when the patient’s condyles are positioned in the joint socket, or what is referred to as the ‘Seated Joint Position’ bite (SJP) (formerly called the ‘Centric Relation Bite’).
CLASS II - SEATED JOINT POSITION
The SJP is the most stable jaw position because the condyles are supported by the inferior articulator eminence, and when the condyles are in this position, the lateral pterygoid muscles should be in a relaxed position, reducing overall muscle activity.
For restorative dentists, prosthodontists and orthodontists, this is the desired treatment position when doing complex dentistry, or when moving teeth. An ideal situation thus occurs when the patient only has one bite - patient’s bite in SJP is the same as their MIP.
For restorative dentists, prosthodontists and orthodontists, this is the desired treatment position when doing complex dentistry, or when moving teeth. An ideal situation thus occurs when the patient only has one bite - patient’s bite in SJP is the same as their MIP.
Write your awesome label here.
TMD Patient Webinar: Dr. Hartlieb reviews the bite of his TMD patient.
For patients that have a disharmony between SJP and CR, the SJP provides a stable position to reduce the muscle coordination necessary when the patient brings their teeth together. However, as the patient’s mandible is seated into SJP, the patient may find that only some of their back teeth touch, with a gap between their front and side teeth. This is the reason that most patients do not want to bite with their condyles seated – they want to bite with as many teeth fitting together as possible.
So, for this reason, patients will activate the appropriate muscles to maximize teeth contacts forgoing joint stability.
Unfortunately, overtime, this reliance on muscle coordination to create a better bite can lead to muscle pain, joint pain, headaches, or other issues that can be disruptive to the patient.
TMJ Splint Therapy for Joint Issues
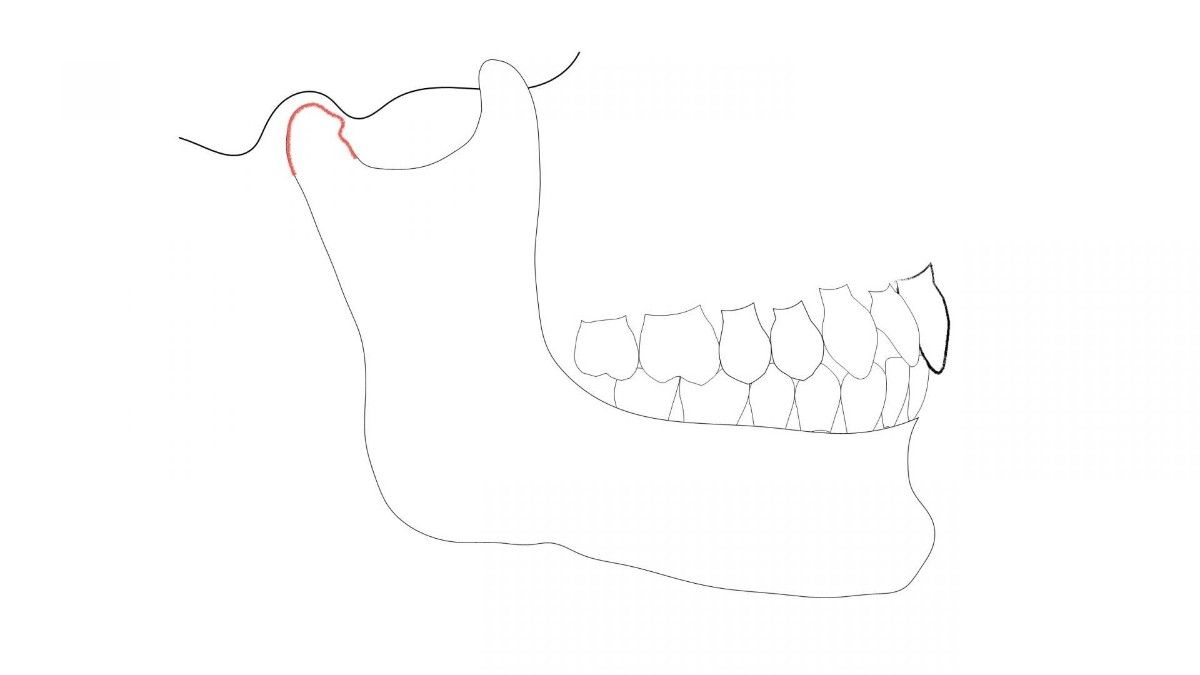
The clicking, or popping, of the disc that is often observed, is due to a stretched ligament (posterior band) that holds the disc in its normal position between the head of the condyle and the inferior articulator surface.
The posterior band can become stretched due to a variety of injuries such as whiplash, trauma to the head, jaw or face, and can be seen with patients that have hyper-laxity in their joints.
While treatment for patients with clicking or popping joints is limited, it is currently believed that a stable bite, and minimizing muscular tension, will minimize the risk of complete disc displacement in the future. Fabrication of a night guard alone can often be insufficient to manage these patients – these are patients that need more comprehensive treatment approach where splint therapy is needed.
Often misunderstood by patients and dentists alike, a night guard is simply a device to separate the patient’s teeth when they are grinding to prevent, or reduce wear on teeth, and to reduce pressures on the teeth and periodontal structures while the patient is sleeping. When appropriately adjusted, these appliances can also serve to reduce muscle tension for these patients.
The posterior band can become stretched due to a variety of injuries such as whiplash, trauma to the head, jaw or face, and can be seen with patients that have hyper-laxity in their joints.
While treatment for patients with clicking or popping joints is limited, it is currently believed that a stable bite, and minimizing muscular tension, will minimize the risk of complete disc displacement in the future. Fabrication of a night guard alone can often be insufficient to manage these patients – these are patients that need more comprehensive treatment approach where splint therapy is needed.
Often misunderstood by patients and dentists alike, a night guard is simply a device to separate the patient’s teeth when they are grinding to prevent, or reduce wear on teeth, and to reduce pressures on the teeth and periodontal structures while the patient is sleeping. When appropriately adjusted, these appliances can also serve to reduce muscle tension for these patients.
Write your awesome label here.
TMD Patient Webinar: Medial pole disc displacement
Splint therapy on the other hand, is treatment with an orthotic to help manage joint or muscle pain for patients with TMD. With splint therapy, as we’ll review later in the blog, repeated adjustments are made to the splint as the muscles of mastication reduce in intensity, and inflammation in the joint space decreases.
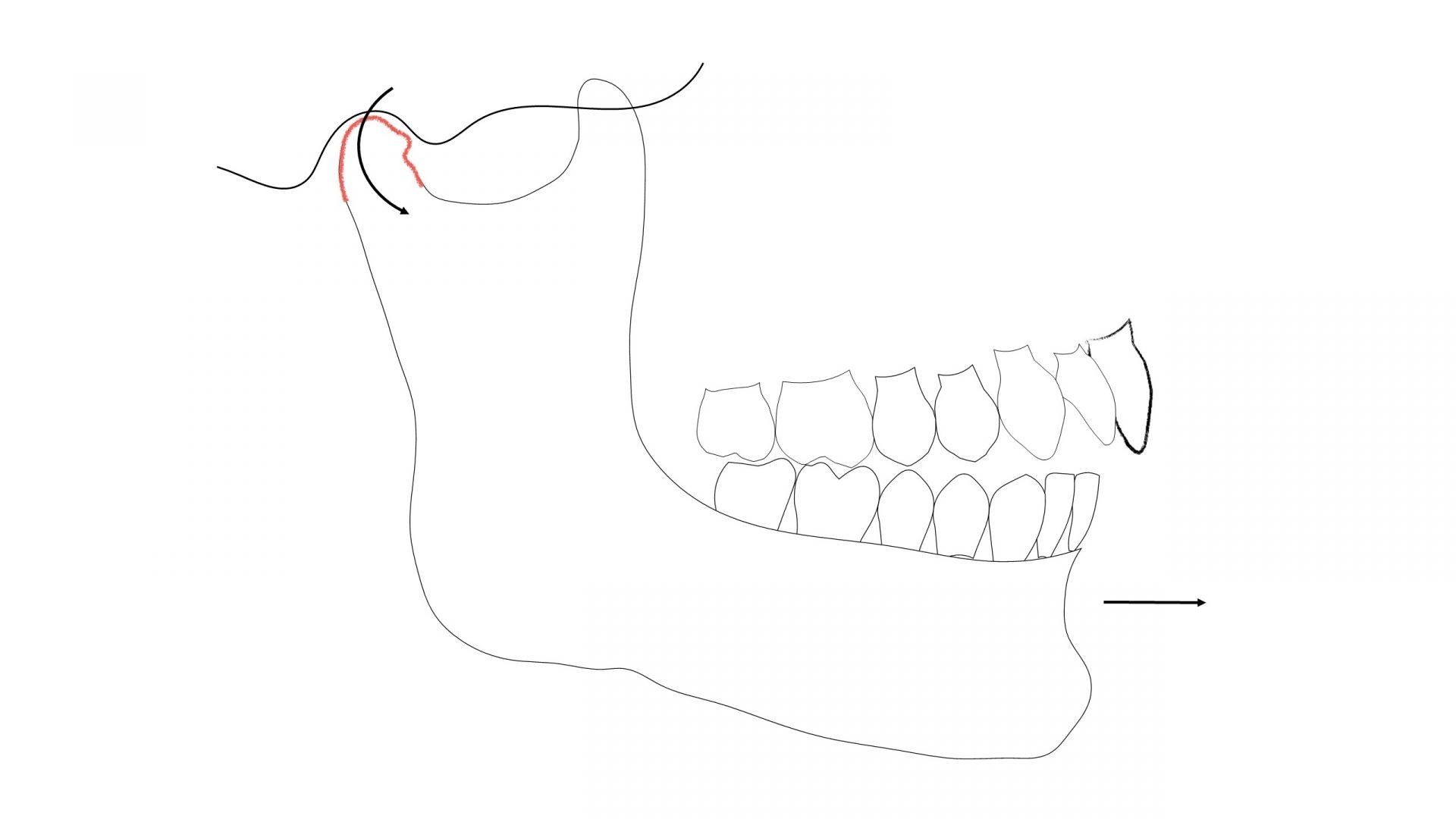
Splint therapy generally takes multiple adjustments of the splint, over many months, at each appointment balancing the splint and eliminating eccentric bite interferences. Many patients will discover that their MIP bite is not in unison with their seated joint position bite as the muscles of mastication begin to relax, and the inflammation in the joint space reduces. This will often present as the CO – CR slide that we learned about in dental school.
Typically, the patient will bite on a posterior tooth when in their seated joint position, and then will ‘slide’ into their maximum intercuspation bite. These ‘slides’ can be managed simply by the continuation of night time splint use, combined with behavioral feedback to minimize daytime tooth clenching. Orthodontics, equilibration or restorative dental procedures may also be considered to provide the patient with a unified bite, where SJP = MIP.
When Does the TMD Patient Require MRI Evaluation?
Write your awesome label here.
TMD Patient Webinar: Lateral pole displacement
For patients with popping or clicking discs, maintaining the disc of the condyle in position is optimal for two principal reasons: first, if the disc is herniated, there will likely be a significant change in the patient’s occlusion, and secondly, with disc displacement, the head of the condyle will now articulate against the opposing bony surface.
The bite change with the disc displacement occurs because there will be a superior seating of the condyle to make up for the space that the disc occupied. If the disc herniates completely, the condyle seats in a superior anterior position, taking up the 3 mm thickness of the disc. There will be an autorotation of the condyle clockwise resulting in the posterior teeth occluding with a lack of contacts with the anterior teeth.
In fact, displaced TM discs should be one of the things to consider in your differential diagnosis when you see a patient with an anterior open bite.
To determine if the TM discs have displaced, an MRI of the joints should be taken. The MRI will indicate if the disc is in the correct position, or if there are perforations, or partial or full displacement of the disc.
Write your awesome label here.
TMD Patient Webinar: How to evaluate the MRI.
When Does the TMD Patient Require CBCT Imaging?
The final area to consider, or the center of the onion if you will, is the bone. For patients that have had long standing disc displacement, and there has been repeated bone rubbing against bone (condyle against the inferior articulator eminence), there is often changes to the bone size, shape and contour.
The patient may experience pain from the bone-on-bone joint relationship, and changes in the bone shape and size will commonly alter bites, causing anterior open bites, canting in the patient’s occlusal plane, and even create facial asymmetries in unilateral condyle breakdown. CBCT imaging of the patient is appropriate to evaluate condyle shape and size.
While the CBCT does not show soft tissue like the TM disc, it can show the relationship of the superior head of the condyle to the inferior articulator eminence. If the condyle is in proximity to the inferior eminence surface, this would suggest that there is a lack of normal space that the disc would typically occupy. However, to get the full picture of the patient TM joint, both MRI and CBCT imaging may be necessary.
The patient may experience pain from the bone-on-bone joint relationship, and changes in the bone shape and size will commonly alter bites, causing anterior open bites, canting in the patient’s occlusal plane, and even create facial asymmetries in unilateral condyle breakdown. CBCT imaging of the patient is appropriate to evaluate condyle shape and size.
While the CBCT does not show soft tissue like the TM disc, it can show the relationship of the superior head of the condyle to the inferior articulator eminence. If the condyle is in proximity to the inferior eminence surface, this would suggest that there is a lack of normal space that the disc would typically occupy. However, to get the full picture of the patient TM joint, both MRI and CBCT imaging may be necessary.
When evaluating a patient with TMD, it’s essential to look at the entire picture, and pull back the layers. It is common that patients with internal joint issues also have muscle issues. The goal of splint therapy is to peel the onion back one layer at a time – first manage the muscles, then determine if splint therapy is able to manage the internal joint issues (disc or bone). Collaborative treatment with physical therapy, chiropractic, pharmacology, and even surgical procedures may be necessary with many of your TMD patients.
Case Study: Does Splint Therapy Work for TMJ?

Sandy was referred to my office by an oral surgeon for generalized facial pain secondary to breakdown of her right TM joint. CBCT imaging demonstrated an atrophic right condyle with significant reduction in shape and size. Sandy states that she has been in moderate discomfort for several years and has noticed a change in her bite – she was no longer able to get her left side teeth together.
Coupled with this unstable bite, Sandy presented with an asymmetrical occlusal plane and a canted esthetic plane.
In our initial consultation, Sandy mentioned that she was also displeased with her smile and would like to investigate treatment to improve her smile after her jaw discomfort was eliminated.
In our discussion related to any relevant history that could be related to her TM joint breakdown, Sandy described multiple car accidents that potentially could be associated with her current situation.
Coupled with this unstable bite, Sandy presented with an asymmetrical occlusal plane and a canted esthetic plane.
In our initial consultation, Sandy mentioned that she was also displeased with her smile and would like to investigate treatment to improve her smile after her jaw discomfort was eliminated.
In our discussion related to any relevant history that could be related to her TM joint breakdown, Sandy described multiple car accidents that potentially could be associated with her current situation.
Write your awesome label here.
TMD Patient Webinar: TMJ evaluation
Concept, to Prototype, to Restoration (CPR) for the TMD Patient
Step 1: TMJ Splint Therapy
The initial phase of Sandy’s treatment was to utilize splint therapy to manage her discomfort. My goal with the splint therapy was to provide Sandy with a balanced bite, using the removable orthotic. A maxillary acrylic, flat-planed splint with minimal anterior guidance was fabricated.
Sandy was directed to wear the splint during sleep, and at any time during the day when she felt that she needed improved bite support.
Over a time period of about 9 months, Sandy presented for multiple splint adjustments.
The time period between appointments was initially approximately 2-3 weeks, but the appointment intervals stretched longer as her clinical signs improved.
Typical of other splint therapy patients, we noted a change in the occlusal markings on the splint at each appointment. The splint would be adjusted for balanced contacts on all teeth, with working side guidance on the anterior teeth and bicuspids, but when Sandy returned at her follow-up adjustment appointment, we would note that splint was no longer balanced, with contacts only on the posterior teeth, especially her right side.
This is a common scenario with TMD patients where the condyle of the damaged joint avoids fully seating into the condylar space due to discomfort.
As the splint is adjusted, the muscles begin to reduce their hypertension, and the inflammation in the joint space reduces.
As the inflammation reduces, the condyle is more easily able to seat into the appropriate supported position. The clinician should observe that the patient’s occlusion becomes more retruded, with more significant imbalance in the bite. In Sandy’s case, the initial contact on the distal right molars became more evident as splint therapy continued.
Write your awesome label here.
BALANCE SIDE INTERFERENCES / WORKING SIDE GUIDANCE
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Splint therapy continues until the patient returns and the balance of the splint is still evident – that is, even and balanced centric contact points have maintained on the splint from visit-to-visit.
Though Sandy was eager to move forward with her dental treatment once she was out of pain and comfortable with her splint, I like to monitor the splint for several months before moving on to restorative treatment.
It should be noted that patients that have displaced TM discs and/or joint breakdown, should be cautioned that bone changes in the condyles overtime should be anticipated. As the bone changes occur, it will be likely that occlusal changes will become evident as well.
Step 2: Create a Balanced Bite
I’m a big believer in taking one step at a time when treating complex care patients; patients with Tmj issues are no exception. Once I have been able to eliminate the patient’s discomfort with splint therapy, it is time to find a way to balance their bite – to mimic the occlusion that they are able to achieve while wearing the splint.
I’m a big believer in taking one step at a time when treating complex care patients
There are 4 ways to create the balanced bite in these cases:
1) orthodontics
2) equilibration
3) restorative addition
4) surgical treatment
In many cases, equilibration of the bite would not be acceptable due to the amount of tooth structure reduction needed to establish a balanced occlusion. Also, it is common that several of these options combined may be needed to provide the patient with an appropriate occlusal scheme.
I reviewed these treatment options with Sandy and discussed the pro’s and cons of each. Sandy stated that she wished to avoid orthodontics and surgery at all costs, but was open to any restorative opportunity to improve her bite and the esthetics of her smile.
1) orthodontics
2) equilibration
3) restorative addition
4) surgical treatment
In many cases, equilibration of the bite would not be acceptable due to the amount of tooth structure reduction needed to establish a balanced occlusion. Also, it is common that several of these options combined may be needed to provide the patient with an appropriate occlusal scheme.
I reviewed these treatment options with Sandy and discussed the pro’s and cons of each. Sandy stated that she wished to avoid orthodontics and surgery at all costs, but was open to any restorative opportunity to improve her bite and the esthetics of her smile.
Step 3: Diagnostic Wax-up & Smile Preview
Write your awesome label here.
TMD Patient Webinar: Smile Preview
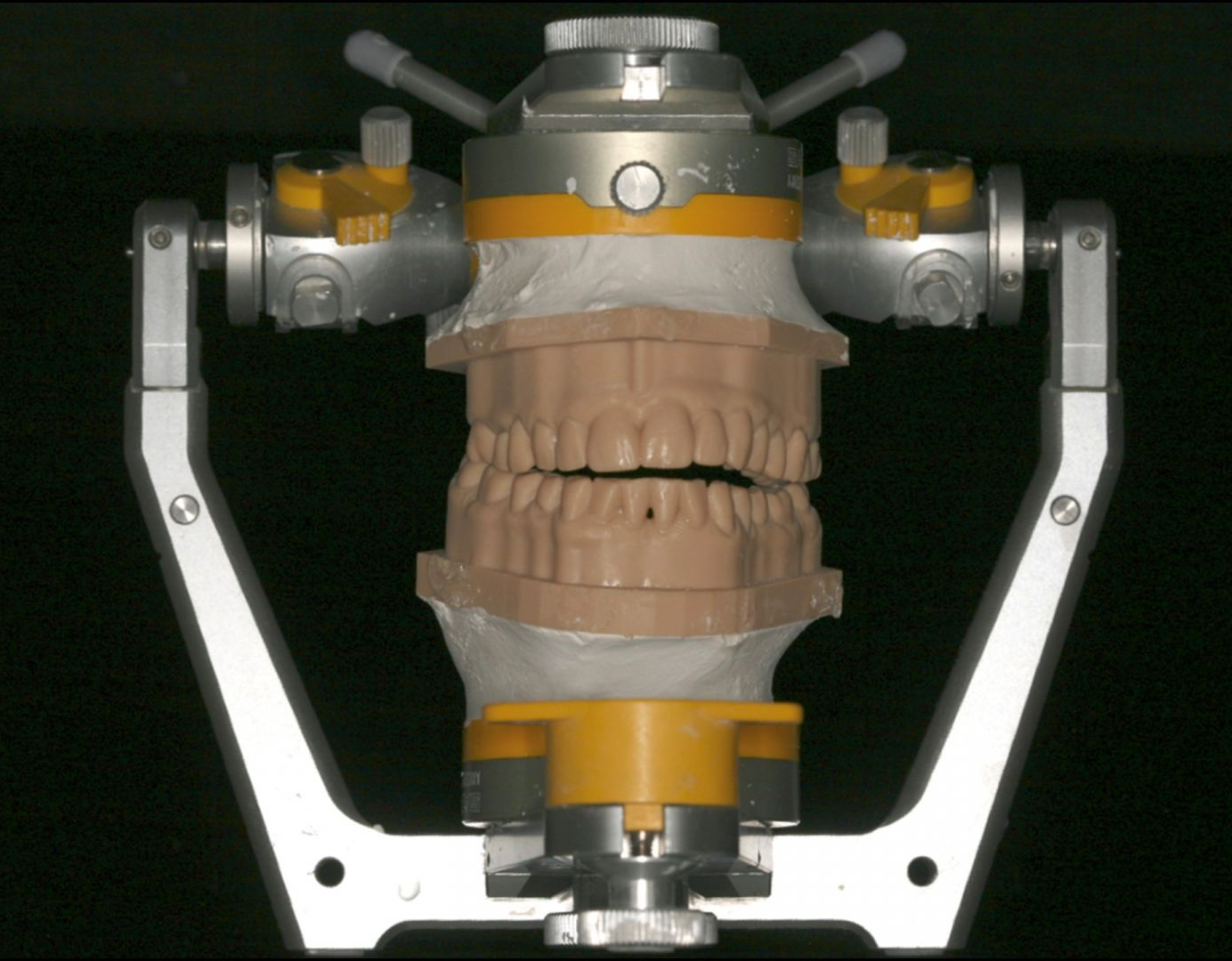
Diagnostic records were taken, including updated photographs, x-rays, intra-oral scanning, SJP bite and a facebow. Sandy’s printed models from her scans were mounted on a semi-adjustable articulator (Sam 3) and a diagnostic wax-up was completed.
The goal of the diagnostic wax-up was to eliminate the cant in her smile (level the maxillary occlusal plane) and to gain occlusal stability in her bite. A putty matrix was created from the diagnostic wax-up to be used for a Smile Preview – a technique that utilizes a crown and bridge temporary bisacryl material to simulate the projected outcome of treatment based on the diagnostic wax-up.
Sandy was able to see the esthetic result anticipated with the proposed treatment and was eager to move forward with the restorative work.

Write your awesome label here.
Write your awesome label here.
Traditionally, dentists would begin the restorative phase of treatment by removing existing crowns and prepping other teeth for the definitive restorations. Provisional crowns would be used as a testing method to test the occlusal, esthetic and phonetic changes created.
In this approach, the dentist and patient are now tied to definitive restorations on these teeth. If the patient does not respond well to the treatment, or there is suddenly a flare-up in the patients TMD, there could be a substantial time period before the dentist can proceed to the final crowns.
Management of patients with temporary crowns on both arches can be complicated if treatment time is extended. Loosening of provisionals with subsequent recurrent caries is an unfortunate, but not uncommon result from extended provisionalization. It is for this reason, and for my patients to budget the costs (and time) of extensive crown and bridge work , that I prefer to utilize non-preparation Prototype Bonding.
Step 4: Prototype Bonding
Write your awesome label here.
TMD Patient Webinar: TMJ splint therapy is complete
With Prototype Bonding, direct resin is used in an ‘additive’ only approach. In the first restorative phase in Sandy’s treatment after the teeth were properly conditioned for the composite, putty guides were utilized (from the wax-up) to create appropriate length and contour for the maxillary arch.
It was necessary to treat the existing porcelain crowns with appropriate etchants and adhesive techniques prior to placing the composite on those teeth. All composite restorations were additive in nature only with no tooth structure removal done at this phase.
A single shade of composite is used to create the ideal shape and contour of each individual tooth, with the final smile design in mind. The second phase of treatment was to bond to the lower teeth, again in this conservative, prep-less approach, to create a stable occlusion.
Following proper etching and adhesive protocols, composite was used to add occlusal and incisal height on the lower dentition to create balanced contacts in MIP, with light anterior and bicuspid disclusion.
Write your awesome label here.
TMD Patient Webinar: New Smile
At a follow-up appointment, the occlusion was further balanced and the esthetic shaping and polishing of the composite was finalized. A new occlusal splint was created though it could be argued that with the new stabilized occlusion, a new splint would not be necessary.
Sandy maintained the prototype bonding for about 8 months. During this time, we evaluated to be certain that the centric contacts were maintaining – that is, there was no observable changes in her occlusion. I explained to Sandy that if we noted changes in her occlusion, it would be better to continue with the prototype bonding than proceed to the final porcelain restorations.
The prototype bonding can be adjusted and added to more easily than porcelain if we were noting a change in her bite. After 8 months of monitoring, we were satisfied that her occlusion was stable and safe to proceed to final restorations.
Managing, not Treating, TM Joint Issues

I treat many patients with TMD in my practice. It needs to be mentioned that there are patients that we are not able to help and do not improve with the splint therapy. We do have a high degree of success however in reducing pain, and improving comfort for our TMD patients.
For many patients, the treatment is limited to splint therapy, and despite having a ‘dual-bite’ (SJP to MIP), they are comfortable, stable, and without pain. They do not wish to have further treatment such as orthodontics, surgery, or restorative work to improve their bite.
Other patients however, wish to have improved balance in their bite, or esthetic improvements in their smile following the splint therapy.
Prototype bonding for these cases has proven to be an effective tool to create balance and stability in patients’ occlusion, while managing esthetic issues.
The prototypes allow for changes and helps patients understand what may, or may not, be achievable with the final esthetic dentistry. The prototype bonding may help patients understand why orthodontics, and/or surgery may be necessary to achieve the patient’s desired outcomes. The prototypes also allow the patient to budget their dental treatment, managing arches, or sections of their mouth at a time, allowing for optimal treatment care over an extended time frame.
Sandy's Final Thoughts
“When I first came in to see Dr. Hartlieb, my smile was totally crooked. I couldn’t bite into a sandwich, and I never dreamed that I could have such a beautiful smile. I could cry. I’m so happy.”
Write your awesome label here.
Drag to resize
Related courses:
→ A New Perspective on Occlusion and TMD with Dr. Jim McKee
→ Reading MRIs - Let's Look Inside
→ The Airway Patient in Your Dental Practice
→ Reading MRIs - Let's Look Inside
→ The Airway Patient in Your Dental Practice
Drag to resize
Dennis Hartlieb, DDS, AAACD
DOT Founder
Share this page
Join 10,000+ dentists who get tips bi-weekly.
Thank you!
By signing up you agree to our Privacy Policy.
Latest from our blog
Our vision is to provide online continuing education workshops and mentorship that are comprehensive for dentists learning at all career levels. DOT is developed for dentists that love to learn online.
CONNECT
Materials Included
Light Brown tints, Enamelize, Unfilled Resin Flexidiscs, Flexibuffs 1/2", #1 artist’s brush, Silicone Polishing Points, IPC Off Angle Short Titanium Coated Composite Instrument
Materials Needed, not Included
- Loupes
Follow along
You are Registered
We’re excited to have you join us! You’ll receive email reminders at with the link to join this event.
If you have any questions in the meantime, feel free to reach out to us at dot@dothandson.com—we’re here to help!
Day 1 (8 - 4 pm CST)
-
Erosion and wear – the why and the how
-
Adding length to teeth – when is it safe
-
Opening VDO to compensate for lost tooth structure – where to begin
-
Records visit and key points you need to understand before you start
-
The smile – the 7 strategic points to consider when evaluating the smile
-
Anterior tooth shape, morphology
-
Clinical case review
-
Upper Putty matrix construction
-
Build lingual incisal wall with putty matrix #6 - #11/ Upper anteriors
-
Full contour build-up #6, #7, #8, #9, #10, #11, shape and polish/ Upper anteriors
Day 2 (8 - 2 pm CST)
-
Who – which patients are candidates
-
Why – explaining to patients the value of the prototype
-
How – step-by-step techniques to maximize predictability, efficiency and success
-
Getting to Yes: conversations with patients about esthetic and reconstructive dentistry
-
The ‘Smile Preview’ – techniques to show the possibilities
-
Lower Putty matrix construction
-
Build lingual incisal wall with putty matrix #22 - #27 / lower anteriors
-
Build-up #22 - #27, shape and polish / lower anteriors
-
Build-up lower occlusal posteriors
-
Demonstration of Smile Preview
Upcoming Virtual Workshops
Write your awesome label here.
December 11 & 12, 2025
CPR for the Worn Dentition (16 CE)
Write your awesome label here.
January 29-30, 2026
Porcelain Veneer Cementation Workshop (14 CE)
Write your awesome label here.
March 27, 2026
Esthetic and Functional Success for Diastema Closure (8 CE)
Write your awesome label here.
May 15, 2026
From Break to Beautiful: Flawless Class IV Resin Restorations (8 CE)
Write your awesome label here.
June 19, 2026
Mastering Intraoral Scanners and Digital Workflow for the Dental Team (4 CE)
Write your awesome label here.
September 25, 2026
Veneering the Dark Central Incisor - Conservative Direct and Indirect Restorative Strategies (8 CE)
Write your awesome label here.
October 30, 2026
3D Printing for the Restorative Dentist
Write your awesome label here.
December 11, 2026
Injection Molding Workshop (8 CE)
Write your awesome label here.
Study Club
Join five in-depth virtual meetings held on Thursday evenings throughout the year. Engage in detailed case presentations, discuss curated research articles, and exchange valuable tips with fellow dentists.
-
01/22/2026
-
04/09/2026
-
06/11/2026
-
10/15/2026
-
12/10/2026
Write your awesome label here.
Coffee & Donuts
Kickstart your Friday mornings with informal sessions and discuss patient treatments, practice management, and receive feedback on your cases.
-
01/16/2026
-
02/13/2026
-
03/20/2026
-
04/10/2026
-
05/08/2026
-
06/05/2026
-
08/21/2026
-
10/09/2026
-
11/20/2026
-
12/10/2026
Popular On-Demand Courses
Write your awesome label here.
Injection Moulding Techniques (3 CE)
Simple, predictable, systematic foundation for you to start your journey with injection moulding
Write your awesome label here.
Advanced Techniques in Composite Veneers (6 CE)
Take control of aesthetic cases in your practice, whether you are enhancing smiles with direct resin veneers or creating provisional restorations for indirect cases.
Write your awesome label here.
A Realistic Perspective on Occlusal Appliances (3 CE)
Learn how to design, fabricate, and manage occlusal appliances with confidence through practical guidance and real clinical case examples.
Write your awesome label here.
Bicuspid Veneer and V-Onlay Preparation (3 CE)
Gain expertise in ‘prep-less’ veneers, buccal cusp reduction, and margin placement methods to enhance your clinical outcomes.
Write your awesome label here.
Class IV Composite Restoration – Polychromatic Approach (3 CE)
This on-demand course covers material selection and advanced layering techniques to help you create natural-looking, long-lasting restorations that set you apart.
Write your awesome label here.
EXOCAD: Foundation (2 CE)
Gain the skills to confidently navigate Exocad, build patient cases, and streamline your workflow using time-saving techniques and presets.
Write your awesome label here.
Class II Direct Resin (3 CE)
Master a reliable approach to Class II restorations by learning how to create ideal proximal contacts that enhance both the strength and aesthetics of your work.
