
Zirconia Bridge Technique: Conservative Esthetic Tooth Replacement
Discover how to use resin cement to secure Zirconia Bonded Bridges and create minimally invasive, esthetic tooth replacement.

It’s Not Your Dad’s Maryland Bridge

Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Three Reasons why the Replacement of Anterior Teeth Might be Necessary:
-
There is an estimated 2% of people born with congenitally missing maxillary lateral incisors1 that need tooth replacement options during their adolescent years.
-
Teeth that have been lost due to trauma, such as cases where the tooth has been completely avulsed, or ‘knocked out.’
-
A tooth that has been lost secondary to previous trauma.
Write your awesome label here.
Write your awesome label here.
These traumatized teeth can manifest with resorptive lesions or peri-radicular breakdown secondary to root fracture.
Write your awesome label here.
Write your awesome label here.
Also, paramount to restorative success is an understanding of the functional and parafunctional tooth contacts as patients use their teeth in their day-to-day living.
Write your awesome label here.
Write your awesome label here.
Removable Treatment Options to Replace the Missing Anterior Tooth
1. Dental Flipper

2. Utilizing a Patient's Invisalign Tray
While all of these options have the advantage of minimizing dental treatment to the surrounding teeth, and the financial investment may be minimized, many patients are unhappy with the challenges of wearing a removable appliance.
Six Potential Challenges Presented by the Removable Prosthesis
- Eating with the
appliance can be difficult as the appliance can ‘move’ during chewing
- Speech may be
affected due to the necessary thickness of the base material necessary to
support the denture tooth (teeth)
- Esthetic Limitations - There are esthetic
limitations of the replacement teeth
- The ‘losability’ of
the appliance – it is not uncommon to hear that a flipper or temporary
removable retainer was accidently thrown out or lost when a patient had left
the appliance out of their mouth
- Uncomfortable - Many patients will
find the appliance uncomfortable and will wear only socially
- Social Limitations - There can be social
issues related to having a missing front tooth. In my 30+ years of dental practice, I have yet to have an adolescent, or an adult, excited to have a removable prosthetic option for their missing front tooth.
Zirconia Resin Bonded Bridges:
Key to Single-Wing Prep Design Success Guide
Key to Single-Wing Prep Design Success Guide
"Fixed" Treatment Options to Replace the Missing Anterior Tooth
For the missing anterior tooth, there are several fixed, or non-removable, options used commonly today.
1. Traditional, or Conventional Bridge

2. Cantilevered Bridge
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Dental implants have evolved as a tremendous opportunity to replace missing teeth with an estimated 450,000 dental implants placed annually around the world.2
Write your awesome label here.
Write your awesome label here.
Limitations of Dental Implants
1. Placement
2. Patients that are Still Growing
The implant tooth will appear shorter at the incisal edges, relative to the other teeth in the smile as the teeth move downward and forward with the facial growth. As a result, the gum line of the dental implant will be more apical, creating an imbalance at the soft tissue level.
3. Age
Recent evidence suggests that dental implants should not be placed in the esthetic zone until a person is in their 20’s, perhaps even into their 30’s because of latent facial growth3.
How the Rochette Bridge Became the Maryland Bridge
The restorative solution, described as a ‘Rochette Bridge”, was a two-winged metal-based bridge that utilized pin holes and retentive preparation designs on the lingual or palatal surfaces of the abutment teeth to support a cemented bridge.
These metal-based tooth replacements where the first step in conservative based dentistry to replace a missing front tooth. With the advent of adhesive dentistry, the Rochette Bridge was transformed and later became better known as the “Maryland Bridge”.
The Maryland Bridge was the first ‘Resin Bonded Bridge’ (RBB) and was developed by Drs. Livaditis and Thompson, from the University of Maryland College of Dental Surgery.
The Maryland bridge design and technique were dependent on utilizing a specific metal etching technique which made the retentive holes, slots, or other preparation features found in the Rochette Bridge unnecessary.
However, there were challenges with the Maryland bridges, including, the shine thru of the metal through the teeth which could make the neighboring teeth look dark, or create a grey, unaesthetic cast to the teeth.

Potential Complications from the Maryland Bridge
One Debonded Wing
Improper Preparation
Occlusal Forces
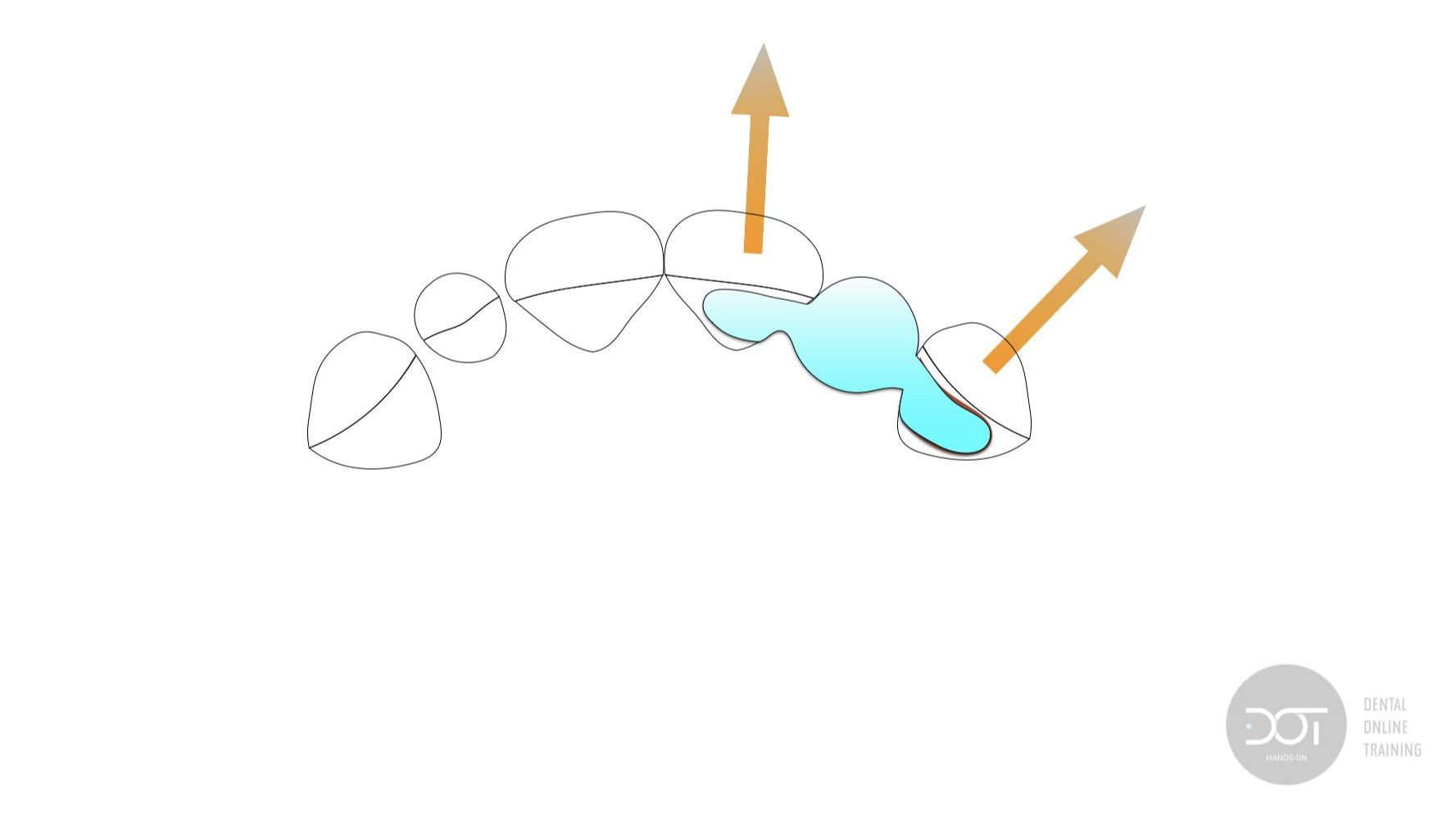
Considering the replacement of a maxillary lateral incisor, during normal function, we would expect occlusal forces to ‘push’ the central incisor abutment tooth in a facial direction. However, in a normal Class I occlusion, the forces on the canine would be more in a lateral direction.
These occlusal forces, being in opposite directions, create tension in the adhesive interface and commonly, with one of the wings debonding from the abutment tooth.
Zirconia Resin Bonded Bridges: Mastering Materials and Cementation Technique Guide

How long do Zirconia Bridges Last?
Write your awesome label here.
Write your awesome label here.
Kern’s 10-year study showed a 91% survival rate demonstrating that these single-winged bonded restorations can be a reliable conservative tooth replacement option for the missing anterior tooth.
While InCeram was an improvement in the strength of tooth colored, non-metal restorative materials, its strength falls significantly short of the zirconia materials available in dentistry today.
Kern noted that none of the bridge failures were related to adhesive failures. Given that our materials and understanding of adhesive bonding is significantly advanced over the last several decades, we should conclude that a single-winged bridge made of a stronger material (zirconia) with improved adhesive techniques should match, or exceed, performances previously recorded.
While single winged bonded restorations may be advantageous in many single tooth replacement situations, two-winged zirconia bonded bridges still may be appropriate when more than one tooth is being replaced, or for treatment considerations when additional restorative treatment is needed on anchoring teeth.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
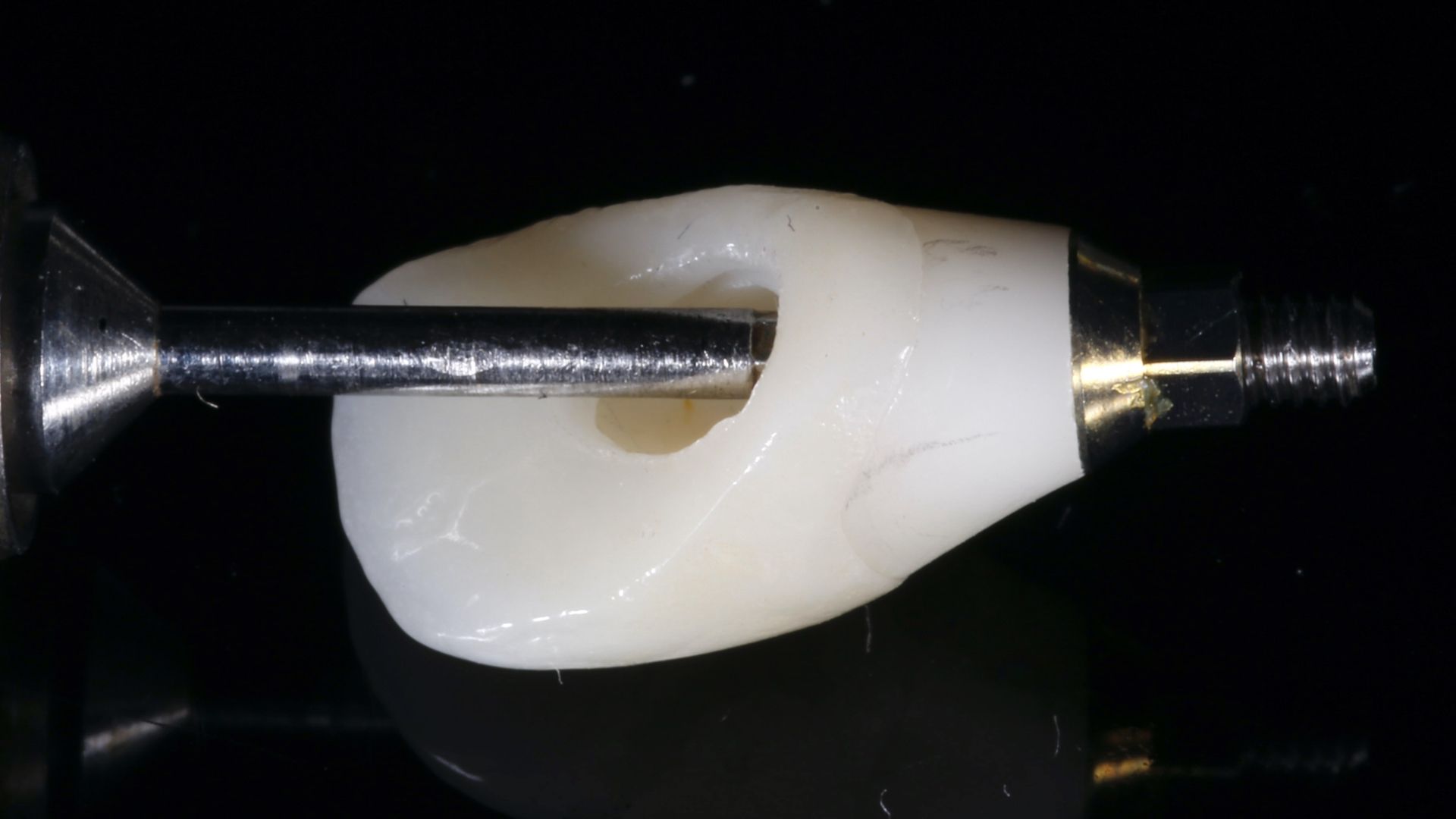
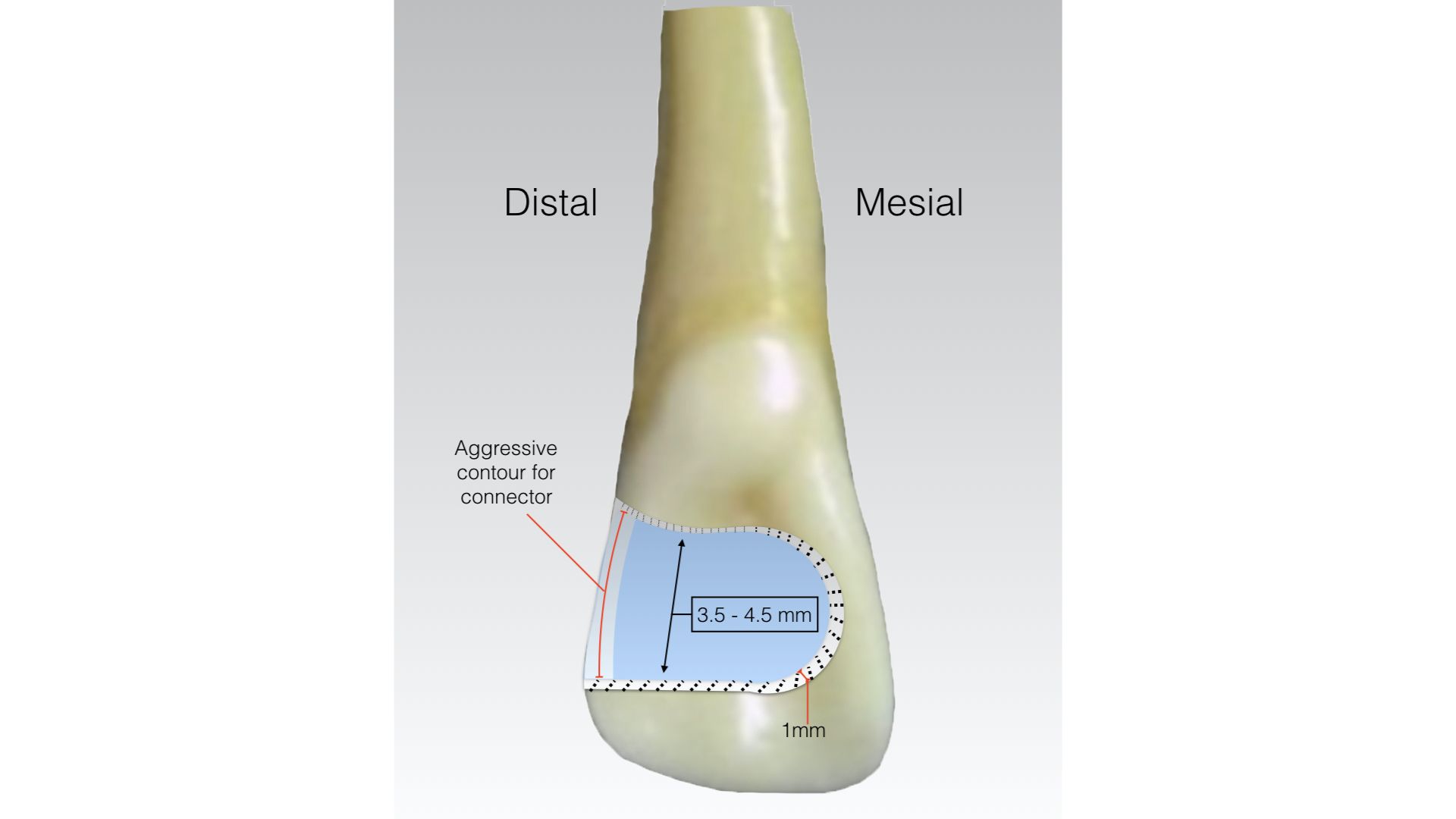
How Thick Should a Zirconia Bond be for Maximum Bondability?
Sillam et al reported in their paper “Influence of the amount of tooth surface preparation on the shear bond strength of zirconia cantilever single-retainer resin -bonded fixed partial denture”5
The shear bond strength to dislodge a 7 mm wide wing had no statistically significant difference compared to a 3.5 mm wide wing. Failures of all the bridges tested were adhesive in nature, with no failure of restorative material reported.
Additional information on zirconia research has demonstrated that the minimal thickness of the zirconia material should be 1.0 mm6. Based on this information, it can be concluded that a retainer wing should be 1.0 mm thick, 3.5 mm from proximal to the cingulum, and about 4.0 mm tall.


APC Protocol for Securing Zirconia Resin Bonded Bridges



How I Use Resin Cement to Secure Zirconia Bonded Bridges
Step 1.
Research has found that the though the dual-cure cements can be cured with only the chemical initiation, light activation has proven to create a stronger resin cement.
Step 2.
After light polymerization, excess cement can be removed with scalers, surgical blades and rotary instrumentation.
Step 3.
It is critical that the connector area is not thinned from adjusting – if necessary, the opposing tooth contact(s) should be adjusted to maintain the 12.0 mm squared thickness of material.
Step 4.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.
Write your awesome label here.

The Zirconia Resin Bonded Bridge Technique:
A Restorative Treatment Option for Patients Missing Anterior Teeth
The restorative replacement of the missing tooth should have minimal tooth preparation and must be esthetic and long lasting. Special attention to preparation design and cementation protocol is critical to the long-term success of the zirconia resin bonded bridge.
Connecting Dentists with Quality, Interactive Dental Training
If you feel strongly about Zirconia Resin Bonded Bridges, join our community and participate in the discussion.
→ Masking the Dark Tooth with Direct Resin
Citations
Dennis Hartlieb, DDS, AAACD
Share this page
Latest from our blog
CONNECT
Materials Included
Light Brown tints, Enamelize, Unfilled Resin Flexidiscs, Flexibuffs 1/2", #1 artist’s brush, Silicone Polishing Points, IPC Off Angle Short Titanium Coated Composite Instrument
Materials Needed, not Included
- Loupes
Follow along
You are Registered
-
Erosion and wear – the why and the how
-
Adding length to teeth – when is it safe
-
Opening VDO to compensate for lost tooth structure – where to begin
-
Records visit and key points you need to understand before you start
-
The smile – the 7 strategic points to consider when evaluating the smile
-
Anterior tooth shape, morphology
-
Clinical case review
-
Upper Putty matrix construction
-
Build lingual incisal wall with putty matrix #6 - #11/ Upper anteriors
-
Full contour build-up #6, #7, #8, #9, #10, #11, shape and polish/ Upper anteriors
-
Who – which patients are candidates
-
Why – explaining to patients the value of the prototype
-
How – step-by-step techniques to maximize predictability, efficiency and success
-
Getting to Yes: conversations with patients about esthetic and reconstructive dentistry
-
The ‘Smile Preview’ – techniques to show the possibilities
-
Lower Putty matrix construction
-
Build lingual incisal wall with putty matrix #22 - #27 / lower anteriors
-
Build-up #22 - #27, shape and polish / lower anteriors
-
Build-up lower occlusal posteriors
-
Demonstration of Smile Preview
Upcoming Virtual Workshops
-
01/22/2026
-
04/09/2026
-
06/11/2026
-
10/15/2026
-
12/10/2026
-
01/16/2026
-
02/13/2026
-
03/20/2026
-
04/10/2026
-
05/08/2026
-
06/05/2026
-
08/21/2026
-
10/09/2026
-
11/20/2026
-
12/10/2026


